Is TMS covered by insurance? This is a common question for many people considering transcranial magnetic stimulation (TMS) therapy, especially those dealing with conditions like major depressive disorder (MDD) or obsessive-compulsive disorder (OCD). In most cases, the answer is yes—TMS is covered by insurance, as long as you meet specific criteria.
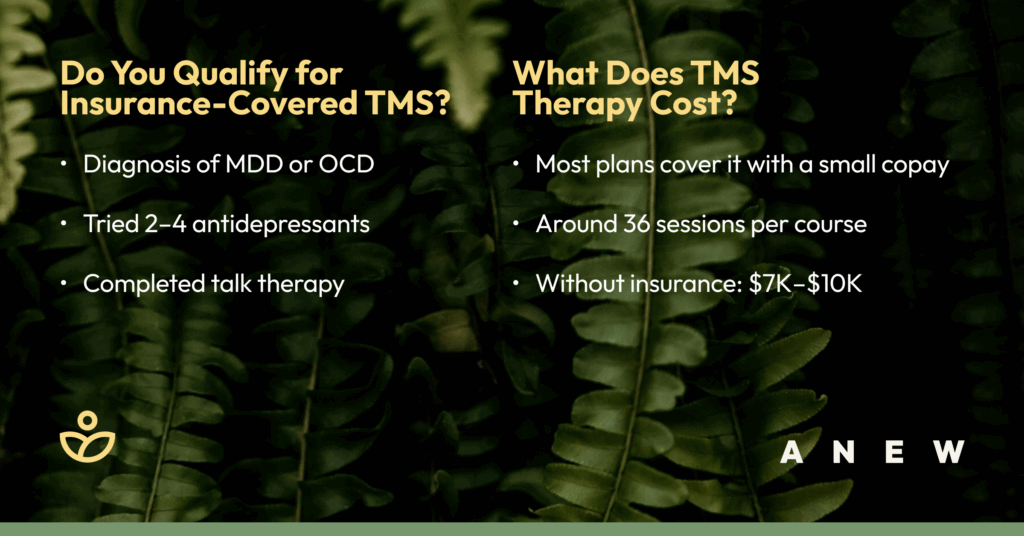
Here’s a quick breakdown of what typically qualifies for insurance coverage of TMS:
- Diagnosis of MDD or OCD confirmed by a licensed professional.
- Previous attempts at treating depression with 2-4 antidepressant medications.
- Attending therapy with a licensed psychotherapist.
Let’s walk through what you need to know to get coverage, understand the costs, and explore alternatives that may also be covered by insurance.
What Is TMS Therapy and How Does It Work?
Transcranial Magnetic Stimulation (TMS) is an FDA-approved, non-invasive treatment for depression and OCD. It works by using gentle magnetic pulses to stimulate specific areas of the brain involved in mood regulation.
TMS is often recommended for people who haven’t found relief with traditional treatments like antidepressants or talk therapy. The procedure is safe, doesn’t require sedation, and has minimal side effects—typically just a tapping sensation on the scalp.At Anew Therapy, we use TMS as part of a personalized, results-driven approach to mental health care. For many, it’s a turning point in their recovery journey.
TMS Insurance Coverage: What to Expect
Transcranial Magnetic Stimulation (TMS) therapy is increasingly recognized as a valuable treatment for mental health conditions like major depressive disorder (MDD). Because of this, many insurance plans now cover TMS—but there are specific requirements to qualify for this coverage.
Who Qualifies for Insurance-Covered TMS?
To be eligible for insurance coverage of TMS therapy, certain criteria must be met:
- Diagnosis of MDD or OCD: A licensed professional must confirm a diagnosis of moderate to severe MDD or obsessive-compulsive disorder (OCD) using DSM-5 guidelines.
- Medication Trials: Patients must have tried and found inadequate relief from 2-4 different antidepressant medications. This demonstrates that traditional treatments have not been effective.
- Talk Therapy: A trial of psychotherapy with a licensed therapist, such as a psychologist or social worker, is typically required. This helps show that multiple treatment avenues have been explored.
Insurance plans may have slight variations in these requirements, so it’s crucial to review your specific policy or contact your provider for detailed information.
How Much Does TMS Therapy Cost?
Because TMS therapy is often covered by insurance, it is an affordable treatment for many. Here’s what you can typically expect:
- TMS with Insurance: Most patients pay a copay or coinsurance per session, which usually ranges from $20-60 for most plans. A full course includes around 36 sessions.
- TMS without Insurance: Without insurance, the total cost for TMS therapy can range from $7,000 to $10,000. At Anew Therapy, we partner with CareCredit to offer flexible financing options and make care more accessible.
Denied TMS Coverage? Here’s What to Do
If your insurance company denies coverage for TMS therapy, don’t lose hope. There are steps you can take to appeal the decision and explore alternative funding options.
- Appeals Process: If denied, work with your TMS provider to gather additional documentation and file an appeal. This might include letters from your doctors and updated treatment records. Persistence is key, as appeals can take time.
- Medical Financing: Consider medical financing options if coverage remains elusive. Some providers offer sliding-scale payment options based on income, making TMS therapy more accessible.
- Explore Alternatives: If TMS remains out of reach, look into other treatments like Spravato, an esketamine nasal spray often covered by insurance, or intramuscular ketamine therapy. Both are effective options for managing depression.
Insurance coverage for TMS therapy can be confusing, but you don’t have to figure it out alone. At Anew Therapy, we’ll advocate on your behalf and work closely with your insurance provider to help you access the care you need.
TMS Insurance Coverage by Provider
While coverage details can vary by provider, many insurers now recognize TMS therapy as a medically necessary treatment for conditions like depression and OCD. Below is a breakdown of how some of the most common insurance companies typically handle TMS coverage.
Aetna
Aetna often covers TMS therapy for major depressive disorder, as long as medical necessity is documented. This usually includes failed trials of antidepressants and psychotherapy. Prior authorization is typically required.
Blue Cross Blue Shield
Most Blue Cross Blue Shield plans provide coverage for TMS when patients meet clinical guidelines, including diagnosis of moderate to severe depression and unsuccessful treatment with standard therapies.
Cigna
Cigna covers TMS therapy for individuals with treatment-resistant depression. You’ll usually need to provide records showing that multiple antidepressant medications and talk therapy have been tried without success.
United Healthcare
United Healthcare includes TMS coverage under many of its plans. Prior authorization and supporting documentation from a mental health professional are generally required to get approval.
DMBA
While DMBA does not explicitly list TMS under standard benefits, it may approve coverage through a prior authorization process. A documented history of treatment attempts is usually necessary.
EMI Health
EMI Health often covers TMS therapy when clinical criteria are met. You’ll likely need to demonstrate medical necessity and submit records showing a history of unsuccessful treatment attempts.
Medicare
Medicare covers TMS for major depressive disorder when specific guidelines are followed. Patients must show that standard treatments have not worked and that TMS is being administered under medical supervision.
Select Health
Select Health typically covers TMS therapy for depression as long as the patient meets specific clinical criteria. Prior authorization and supporting documentation are usually required.
When Insurance Won’t Cover TMS: Your Options
Some insurance companies, especially smaller or less comprehensive plans, may not cover TMS therapy. If you’re not covered, CareCredit is a great option for financing your mental health treatment. It offers flexible monthly payment plans that can make TMS more affordable. At Anew Therapy, we’re happy to walk you through your payment and financing options so cost isn’t a barrier to care.
Finding the Right Treatment Plan at Anew Therapy
At Anew Therapy, we know that traditional approaches to depression, OCD and anxiety don’t work for everyone. In fact, up to 85% of people don’t find relief with standard medications or talk therapy alone. That’s why our clinic specializes in innovative mental health treatments like TMS, Spravato, and ketamine therapy—bringing the future of mental health care to Utah.
Whether you’re just starting your mental health journey or feeling stuck with treatments that haven’t worked, Anew Therapy offers personalized care backed by science and compassion. We’ll help you navigate your insurance coverage for TMS or ketamine treatment and guide you toward the option that fits your needs.
You don’t have to keep searching for solutions. With Anew Therapy, you’re in expert hands—and you’re not alone. Schedule your free evaluation today and discover a treatment plan that actually works.

Searching for the best TMS clinic in Utah? Anew Therapy offers expert care and proven results. Schedule your free evaluation today.